It’s a scary proposition, major surgery, when you have conditions like fibromyalgia and chronic fatigue syndrome. When I knew I would need the surgery, I began to look for other’s experiences so I could gauge what I might be able to expect. It was hard to find stories that could resemble mine.
So I took copious notes throughout my process so that I could share them with you.
I had endometriosis excision and hysterectomy in June 2023.
Brief backstory: I have had heavy and painful periods for my whole menstruating career. I’d done the dance with birth control. But for the previous year the pain was escalating exponentially. The period pain was excruciating, I could not function through it, and nearly went to the hospital a few times. The off-period pain was beginning to significantly impact my quality of life. I was struggling.
Due to the public system being overwhelmed here in New Zealand, we had to go privately to be seen. And I am so glad that I did. I can’t imagine what I would have endured for months or years more of that situation.
Preparation
Prior to surgery I did my best to prepare my body to be as healthy as possible. But that ship really had sailed. I was struggling. I was burnt out from trying to manage. One thing I did do was amp up my nervous system practices.
Pre Op
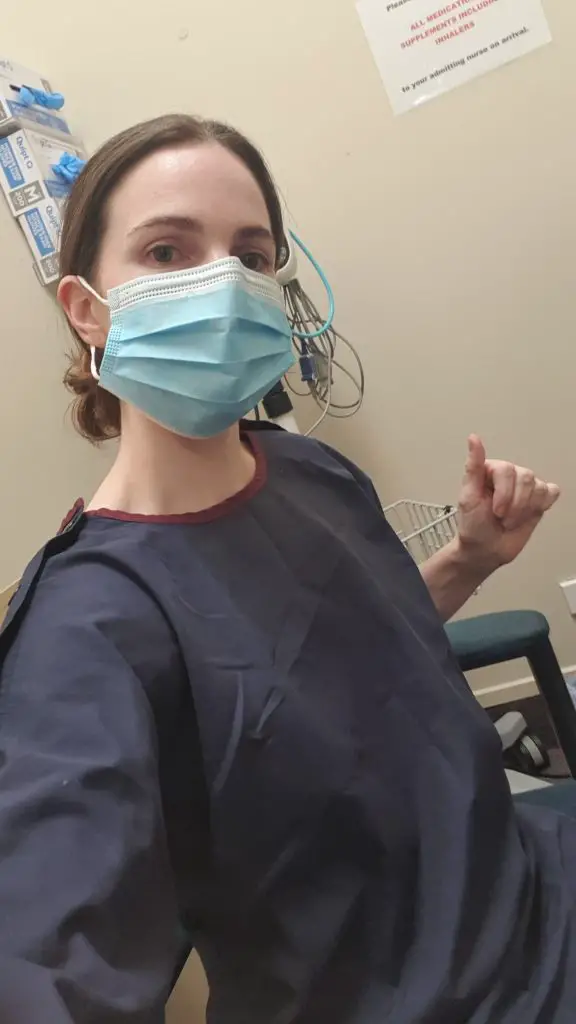
The morning of surgery went really smoothly. I ensured that I only needed to get up, get dressed and leave. So there was no time to fuss about being hungry or not having coffee. We saw the sunrise as we drove to the hospital. I was whizzed through the pre op processes relatively quickly. For which I am grateful.
I tried to let everyone I met know about my sacroiliac joint dysfunction and ask them to be mindful of moving my legs when I was unconscious. Unfortunately I think lying on the flat operating table for 1.5 hours was too much for my poor lower back/pelvis. More about that in a bit.
When I was wheeled into the operating theatre it was a bit overwhelming to see all of the people there. Fortunately I didn’t survive the relaxing medicines they gave me to keep me calm. I don’t remember seeing a gas mask or anything. I was just out.
Waking up
Waking up was not the most pleasant experience of my life. Despite following instructions from my anesthesiologist and the LDN Research Trust, the low dose Naltrexone hadn’t fully cleared from my receptors. So the morphine wasn’t working properly. I woke in agony.
I could hear my heart rate monitor going off, my mid section was burning and an alarm went off every few minutes so the nurse could administer medicine into my IV line. It would have been rather traumatising except for two things. One the nurses who looked after me was so lovely. One held my hand for a time. And the second was my breath. I hunkered down and focused on keeping my breath slow and controlled.
Eventually I was declared stable enough to go to the ward.

The first night
Despite having a pain pump, I was in a lot of pain. There were times when I was sure it had been more than five minutes since my last pain dose, but when I pressed the button it wasn’t time! I couldn’t open my eyes, I was too fatigued. So I had nothing to do but experience my body. It was a rough night. I had a blood pressure, heart rate and oxygen machine on. I couldn’t get to sleep, if I did sleep it was in super short, light chunks. The alarms on the machines kept going off. Nurses assistants couldn’t figure it out and eventually they just turned them off!

The next day
They removed the catheter at 6am. I spent the entire morning trying to go to the toilet. I needed to desperately. But it wasn’t happening. When they checked how much urine was being stored up in my bladder, they decided I needed a catheter again.
That turned out to be a good idea. The 12 hours of rest, including decent sleep that night, helped me to wake the next day fresh.
What they found
Endometriosis, in one main area. The uterus didn’t show signs of why it was so mad, but the surgeon said there must have been something. The uterus, fallopian tubes and cervix are gone. The ovaries were freed from their position and lifted out of the way. The hope is that they won’t fail. Unfortunately early failure of ovaries after hysterectomy is not a low figure. We will see.
Pain relief
I don’t seem to feel nice on the opioid medicine. It made me very sleepy, brain foggy and hardly able to open my eyes. So when they took out the pain pump, I worked with the nurse to stagger the medication so that we covered the pain but reduced the effects,
On the day I went home they sent me with Gabapentin, diclofenac, codiene and paracetamol. When I looked up Gabapentin online, I saw that it had a moderate reaction with quetiapine. So I chose not to take that. A proven medicine that helps me is the priority.
On the second day home I found that the diclofenac wasn’t going down well for me either. So, on my surgeon’s advice, I switched to Ibuprofen. I chose not to take the codeine as I wanted to clear my receptors and go back on LDN in the near future.
So I was rigid with my paracetamol and ibuprofen dosing. I rested. Used my heat pack religiously. And got through. I’m not suggesting you should. I made a decision to prioritise medicines that I know help me a lot.
Poop and Gas
After endometriosis excision surgery one is usually filled with gas so that they can more easily find the endometriosis. Your bowels and systems also get sluggish from all the medicines.
I had gas from the beginning, it was quietly working it’s way through my system, with some discomfort.
I spurred it along with a lot of diaphragmatic breathing and kept my body moving, even when I couldn’t get up. I did toe points, calf stretches and arm stretches.
A couple of days of laxatives and some considerable discomfort saw me make my first bowel movement. And I was away laughing. So thankfully I got off lightly there.
The gas pains in my chest and upper back was worst on the second day but I basically lay where with many heating pads all over my body.
Sacroiliac Joint Dysfunction
Unfortunately from the time I woke up, my low back was very sore. The low back was very put out from lying flat on the operating table and being handled without my conscious guidance. So for the first month and counting, it’s been more of an issue than the incisions. The incisions have healed rather well and as long as I was mindful of movement, weren’t too bad. But the low back, man! I used my heating pad from the first day. Did a very micro pelvic tilt from the third day. And full cat and cow from the fourth week. Mobilizing helps.
Sleeping Positions
I found that sleeping with my upper body elevated was best for the first few days. After that I found it better to elevate my legs higher. I usually sleep with one pillow under my knees for my lower back, as above. However, I found two pillows really helped take the pressure off my incisions and lower back. So it was like I slept in “legs on a cushion” pose, an adapted version of legs up the wall that I love. Over time, I slid the second pillow down so the incline was less and less. But I continued to use two pillows even at four weeks post op.
Fatigue
Besides the lower back pain, the fatigue was also flared post op. Understandably. But so was the orthostatic intolerance. My heart rate would shoot sky high from basically nothing. I could be standing in the lounge, and all of a sudden it would climb up. So I would have to sit down and breathe the heart rate down. This did help guide me through those early weeks so that I couldn’t overdo it. At week four it was settling down. My heart rate would rise during activity, but it wouldn’t make me feel sick or dizzy. Progress.
Read more about Using a Fitbit to Manage My Health

Four Weeks Summary – Hysterectomy and Endometriosis Excision
I am so thankful that it is done. I am so happy I got it. Our family has made sacrifices for it to happen. But I can’t even think of what it would be like to let it go on like that.
One week post op is when I would have been due for my next period. I was in less pain one week post op than I would have been if I had had the period! The is mind-blowing.
If you have heavy and/or painful periods. Please don’t let anyone fob you off. It may not be endometriosis, but it is not normal for such painful periods that you can’t take an ibuprofen and get on with your day – my surgeon said this!
I can’t wait to see how my body goes as I heal. My surgeon expects that some of my fatigue should reduce without the inflammation of the endometriosis and without the heavy and painful periods each month. I hope that the reduction in pain, fatigue and stress will have a positive flow on effect for my entire situation. I will keep you updated!
